52 YEAR OLD MALE WITH ABDOMINAL DISTENSION
Kausalya Varma, Intern
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
52 YEAR OLD MALE WITH ABDOMINAL DISTENSION
CHIEF COMPLAINTS:
A 52 year old male came with the chief complaints of fever and chills since yesterday night and distension of abdomen since today afternoon. He also has complaints of decreased urination since today afternoon.
HISTORY OF PRESENTING ILLNESS:
- Patient was apparently asymptomatic 1 day ago, after which he developed fever which was low grade, 1 episode, associated with chills, subsided on medication.
- He has complaints of distension of abdomen since today afternoon which was insidious in onset, gradually progressing, associated with mild lower abdominal discomfort and has no aggravating or relieving factors. Patient has been passing flatus. Patient passed stools- 2 episodes since 6pm today.
- He also had complaints of decreased urination since today afternoon.
- H/O sudden weakness of all four limbs (lower limbs>upper limbs) since the afternoon.
- H/O trauma to the neck (after a fall post alcohol intake) 2 years back. He suffered a traumatic spinal cord injury with a C5-C6 laminectomy and lateral mass fixation.
- Patient received physiotherapy. He has had a regular change of foleys catheter every 15 days since 2020
PAST HISTORY:
- H/O similar complaints of mild abdominal distension- 2 episodes in 2020
- H/O use of Tab Baclofen 10mg daily since 2020
- Not a K/C/O DM, HTN, asthma, epilepsy or CKD
GENERAL EXAMINATION:
The patient was conscious, coherant, and co-operative and well oriented to time, place and person. With prior consent, patient was examined in a well lit room, lying down on the bed. She in well built and well nourished.
Pallor- Present
Icterus- Absent
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
Koilonychia- Absent
VITALS-
(At admission)
Temperature- 100.5
Pulse rate- 96 bpm
Blood pressure- 90/60 mmHg
Respiratory rate- 34 cpm
GRBS- 145mg/dl
Sp02 at room temp- 90%
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM-
Inspection-
Chest is bilaterally symmetrical
The trachea is positioned centrally
Apical impulse is not appreciated
Chest moves normally with respiration
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt in the midline
Chest moves equally on both sides
Apical impulse is felt in the fifth intercostal space
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
Auscultation-
Normal in all areas
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 2 cm away from the midclavicular line
No parasternal heave or thrills are felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
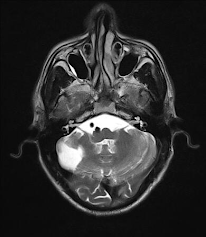
CENTRAL NERVOUS SYSTEM-
Pupils- left- dilated non reactive to light
right-NSRL
Higher mental functions
- Conscious
- Oriented to time,place and person
- Memory - Intact
- Speech - no deficit
Cranial nerve examination
• 1 - olfactory sense - normal
• 2- visual acuity present,direct reflex R L
+ -.
Indirect reflex + -
• 3,4,6 - no ptosis Or nystagmus
• 5- corneal reflex present
• 7- no deviation of mouth, no loss of nasolabial folds, forehead wrinkling present
• 8- Decreased hearing
• 9,10- position of uvula is central ,Gag reflex- present
• 11- sternocleidomastoid contraction present
• 12- no deviation of tongue
Motor system
Reflexes
Right Left
Biceps 3+ 2+
Triceps 3+ 2+
Supinator 2+ 2+
Knee. 2+. 2+
Ankle. 1+. 1+
Plantars- extensor extensor
Power. Lt. Rt
Upper limb -5/5. 5/5
Lower limb -3/5 3/5
TONE. Lt. Rt
Upper limbs N N
Lower limbs N increased
No Involuntary movements
SENSORY SYSTEM
I – SPINOTHALAMIC R L
1. Crude touch N N
2. Pain. N. N
3. Temperature. N. N
II – POSTERIOR COLUMN
1. Fine touch. N. N
2. Vibration. N. N
3. Position sense. N. N
4. Romberg’s sign -Negitive
III – CORTICAL
1. Two point
discrimination. N. N
2. Tactile localisation. N. N
3. Graphaesthesia. N. N
4. Stereognosis. N. N
CEREBELLAR Tests
No Nystagmus
Finger Nose test - normal
Heel Knee test - normal
Dysdiadokokinesia - normal
PROVISIONAL DIAGNOSIS-
Paralytic ileus secondary to hypokalemia
True Hyponatremia (Hypotonic Hyponatremia)
S/P C5-C6 laminectomy 2 years back
TREATMENT-
IV fluids NS,RL @75ml/hr
Inj taxim 1g IV BD
Inj Optineuron 1amp IV in 100ml NS IV OD
Tab PAN 40mg PO OD
Tab DOLO 650mg PO SOS
Proctosedyl ointment for L/A
Syp Cremaffin 15ml PO OD
Strict vital monitoring 4th hourly and inform SOS








Comments
Post a Comment