35 YEAR OLD FEMALE WITH FEVER AND HEADACHE
Kausalya Varma, Intern
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
35 YEAR OLD FEMALE WITH FEVER AND SEVERE HEADACHE SINCE THE LAST 1 WEEK
A 35 year old female resident of nakrekal who is a house maker by occupation came with
Chief complaints-
1.Fever since 1 week
2.Headache since 1 week
History of presenting illness-
Patient was apparently asymptomatic 1 week back then she developed fever which is intermittent in onset(on and off),increasing at night time and decreasing in the morning,associated with chills and headache.
Fever is relieved by taking antipyretic.No history of Nausea,vomiting,rash or body pain.
History of unilateral headache since 1 week which is severe throbbing type in left fronto parietal occipital region radiating to the neck,it is aggravated on exposure to stress.Headache makes her wake up abruptly in the night leading to inadequate sleep.
Headache is associated with vomiting(just 1 episode),phonophobia and blurring of vision(history of change in spectacles),decreased regular physical activity,tingling sensation in hand and feet.It relieves on taking rest and medication.No history of aura,photophobia,depression,irritability,cravings,diarrhoea/constipation.
She has history of burning micturition since 5 days associated with decreased urine output,decreased frequency,left loin pain which is dragging type pain(since 2 days).No aggravating and relieving factors.No history of urgency,hematuria,nausea,vomiting.
Daily routine-
She gets up at around 5 AM in the morning,does her daily chores and helps her children get ready for school.She has her breakfast at 8.30 AM in the morning and then sleeps for sometime before preparing and eating lunch by 2 pm.She spends rest of her day by watching TV or doing daily chores.She used to work as a daily wage labourer before 6 years.
PAST HISTORY-
Similar episode one year back.
Not a known case of diabetes mellitus,hypertension,epilepsy,cardiovascular disease and tuberculosis.
History of hypothyroidism 10 years back.She was taking 50 mg thyroxine supplements until 2 years before when she had few episodes of lethargy and she had to consult a local doctor who investigated her thyroid profile and increased thyroxine dose to 75 mg thyroxine supplements.
History of renal stones in the left kidney 6 years back for which she took some conservative treatment.
Family history-
No significant family history.
Personal history-
Diet: mixed
Appetite: decreased
Sleep: Inadequate
Bowel and bladder: constipated
Addictions: none
No H/O of any drug allergy.
General examination-
Patient is conscious,coherent and cooperative.Well oriented to time,place and person,Moderately built and nourished.
O/E-Thyroid appears normal
Clubbing-absent
Cyanosis-absent
Icterus-absent
Pallor-present
Generalised lymphadenopathy-absent
Edema-absent
Fever chart-
Vitals:
Temperature-99 F
PR-84 bpm
RR-20 cpm
BP-100/70 mm of Hg
Systemic examination:
CVS- S1 S2 heard,no murmurs present.
RESP- bilateral Air entry present
Normal vesicular breath sounds heard
ABDOMEN-
Examination of oral cavity is normal
Inspection::
Shape-normal (rounded)
No flank fullness is seen
Skin-no scars seen,presence of striae
No dilated veins seen
Movements of abdominal wall-no visible peristalsis,no visible pulsations
Umbilicus-inverted
PALPATION::
No tenderness
Warmth-present(fever)
Rigidity,guarding is absent
No organomegaly,normal bowel sounds heard
CNS-no focal Neurological deficits found
Higher mental functions-normal
Brudzinski’s sign-Absent
Kernig’s sign-Absent
Provisional diagnosis:-
Migraine/left renal calculi/UTI
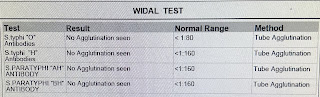
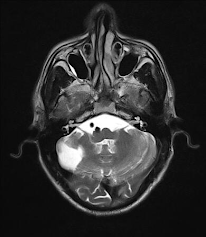
Investigations:













Comments
Post a Comment