A 52 year old male with Cerebellar Ataxia
Kausalya Varma, MBBS 8th semester
Roll no: 59
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 52 YEAR OLD MALE WITH CEREBELLAR ATAXIA
Following is the view of my case (history as per date of admission):
CASE:
A 52 year old male came to the hospital 2 days back presenting with slurring of speech and deviation of mouth that lasted for 1 day and resolved on the same day.
HISTORY OF PRESENTING ILLNESS:
- Patient gave a history of giddiness 7 days back. It started at around 7 am when the patient was doing his usual morning routine. He suddenly felt giddy and took rest, after which it subsided briefly. This was associated with 1 episode of vomiting on the same day.
- Patient was asymptomatic for 3 days, after which he consumed a small amount of alcohol.
- He then developed giddiness, that was sudden in onset, continuous and gradually progressive. It increased in severity upon getting up from the bed and while walking.
- This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
- He has associated vomiting- 2-3 episodes per day, non projectile, non bilious containing food particles.
- Patient has H/o postural instability- he is unable to walk without presence of supports, swaying is present and he has tendency to fall while walking
- No diplopia, dysphagia, dysarthria
- No H/o any seizure like activity.
PAST HISTORY:
Medical History- Patient was found to have denovo HTN, and he did not continue taking medication regularly.
No history of DM
Surgical History- No relevant surgical history.
PERSONAL HISTORY:
GENERAL EXAMINATION:
The patient was conscious, coherant, and co-operative and well oriented to time, place and person. He is sitting comfortably on the bed, moderately built and well nourished.
Pallor- Absent
Icterus- Absent
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
VITALS-
Temperature- Afebrile
BP- 130/100
Pulse- 100
Respiratory Rate- 20
Oxygen saturation- 97% on room air
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM- Normal vesicular breath sounds heard
CVS- S1 and S2 heard, no added murmurs
PER ABDOMEN- Soft and tender, No organomegaly
CNS-
- No sensory symptoms are present
- Motor system examination:
RIGHT LEFT
TONE
Upper limb Normal Normal
Lower limb Normal Normal
POWER
Upper limb 5/5 5/5
Lower limb 5/5 5/5
REFLEXES +2 +2
GAIT- Waist based- Ataxic gait
CRANIAL NERVES-
- Tests for VIII nerve (vestibulocochlear): Rinnes test- Right ear: BC>AC, Left ear: AC>BC
Webers test: No lateralisation
NYSTAGMUS- Bilateral horizontal nystagmus, vertical upbeat nystagmus, more on right lateral position with a fast component to the left.
PROVISIONAL DIAGNOSIS:
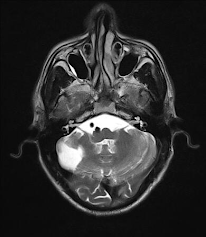
Cerebellar Ataxia secondary to Acute Cerebrovascular Accident (CVA) with infarct in the right inferior cerebellar hemisphere.
TREATMENT HISTORY:
Tab Veratin 8 mg PO TID
Inj Zofer 4 mg IV/TID
Tab Ecosprin 75 mg PO/OD
Tab Atorvostatin 40 mg PO/HS
BP monitoring- 4rth hourly
Tab Clopidogrel 75 mg PO/OD
Inj Thiamine 1 AMP in 100 ml NSPO/BD
Tab MVT PO/OD
ADVICE ON DISCHARGE-
Tab Vertin 8 mg PO TID - 1 week
Tab Zofer 4 mg IV/TID - 1 week
Tab Ecosporin 75 mg PO/OD - 1 week
Tab Atorvostatin 40 mg PO/HS - 1 week
Tab Clopidogrel 75 mg PO/OD - 1 week
Tab MVT PO/OD - 1 week
FOLLOW UP-
Review to OPD after 10 days
QUESTIONS:
1) Did the patients history of denovo HTN contribute to his current condition?
2) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Under the guidance of Dr. Vamshi and Dr Rashmi



Comments
Post a Comment