MEDICINE BLENDED ASSIGNMENT- MAY 2021
MEDICINE BLENDED BIMONTHLY ASSIGNMENT (MAY)
I have been given the following cases to analyse and solve, in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and to comprehending clinical data including history, clinical findings, investigations and diagnosis, and then come up with a treatment plan.
This is the link of the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the medicine assignment based on my comprehension of the cases, divided as per the system concerned:
1) PULMONOLGY
CASE A
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Q1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS. Timeline-
|
Jan, 20 yrs ago |
·
Her
first SOB episode ·
Lasted
one week ·
Relieved
on taking medication |
|
Jan, 19 years
ago Jan, 18 yrs ago Jan 17 yrs ago Jan, 16 yrs ago Jan, 15 yrs ago Jan, 14 yrs ago Jan, 13 yrs ago |
·
Similar
episodes ·
SOB
lasted approximately one week ·
All
episodes were relieved upon taking medication |
|
Jan, 12 yrs ago |
·
Lasted
20 days ·
Episode
of SOB ·
Hospitalised ·
SOB
decreased upon treatment in the hospital |
|
Jan, 11 yrs ago Jan, 10 yrs ago Jan, 9 yrs ago |
·
SOB episodes ·
Lasting
almost a month |
|
8 yrs ago |
·
Polyuria
( diagnosed as DM) ·
Diagnosed
with diabetes |
|
Jan, 7 yrs ago Jan, 6 yrs ago Jan,5 yrs ago |
·
SOB
episodes ·
Lasting
almost a month |
|
5 yrs ago |
Treated for
anemia with iron injections |
|
Jan, 4 yrs ago Jan, 3 yrs ago Jan, 2 yrs ago Jan , 1 yr ago |
·
SOB
episodes ·
Lasting
almost a month |
|
30 days ago |
·
Latest
episode of SOB ·
SOB
was insidious in onset and gradual in progression Initially
SOB occurred on exertion and was relieved upon rest ·
Generalised
weakness( administered IV fluids by a local rmp) |
|
20 days ago |
·
Patient
got HRCT done outside which showed signs of bronchiectasis ·
Diagnosed
with hypertension |
|
15 days ago |
·
Pedal
edema upto ankle, pitting type ·
Facial
puffiness |
|
2 days ago |
·
SOB
at rest (grade 4) and was not relived with nebulisers ·
SOB
progressed (the
patient’s SOB is usually relieved with the use of nebulisers and inhalers but
that did not happen in this episode) ·
Drowsiness ·
Decreased
urine output |
Anatomical location - Lungs and the airway
Etiology- Primary etiology may be the the occupation of the patient. The patient works in a paddy field which increases the risk of being exposed to fine dust. Prolonged exposure to the dust can cause COPD. The pateint has findings of bronchiectasis.
Q2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS. 1) Head end elevation 30-45°
It is recommended in this patient
since she is on mechanical ventilation, to reduce the incidence of Ventilator associated pneumonia that occurs due to aspiration of contaminated
oropharyngeal secretions following endotracheal tube intubation.
Efficacy based on studies: Moderate quality evidence from eight studies involving 759 participants demonstrated that a semi-recumbent (30º to 60º) position reduced clinically suspected VAP by 25.7% when compared to a 0° to 10° supine position.
2) O2 inhalation-
It is given for this patient as her spo2 levels at the time of presentation were 75% at room air
Indication- Supplemental o2 therapy given when spo2 levels are below
<92% at room air.
3) Intermittent BiPAP-
Bilevel positive airway pressure (BiPAP) ventilation is a technique used to provide support to a spontaneously, but insufficiently, breathing patient using a nasal mask.
MOA: BiPap machine supplies pressurized air into your airways. It is called “positive pressure ventilation” because the device helps open your lungs with this air.
Indication: it is given to the
patient to provide respiratory support as she is diagnosed with COPD.
4) Injection Augmentin 1.2gm IV/BO
It is given to the patient to treat Bronchiectasis.
Augmentin is a combination of
Amoxicillin- binds to penicillin binding proteins in bacterial cell wall and thereby inhibits bacterial cell wall synthesis.
Clavulinic Acid - is a beta lactamase enzyme inhibitor , thereby
facilitates action of Amoxicillin.
5) Tab. Azithromycin 500mg OD
It is given to the patient to provide symptomatic relief and reduce
incidence of acute exacerbations of COPD.
Efficacy- A randomized controlled trial found that patients hospitalized for an acute exacerbation of chronic obstructive pulmonary disease (COPD) experienced reduced rates of treatment failure when adding azithromycin to their standard of care.
6) Inj Lasix IV BO
If SBP greater than 110 mmHg
It is given to the patient to
relieve symptoms of fluid retention (edema)
It is also used to treat
hypertension
MOA: Furosemide(LASIK) acts by inhibiting the luminal Na-K-Cl cotransporter in the thick ascending limb of the loop of Henle, increases the excretion of Na+ and water by the kidneys, thus increasing urine output.
7) Tab Pantop 40mg PO OD
Indicated due to the patient being on antibiotics.
8) Inj Hydrocortisone 100 mg IV
It acts by reducing inflammation in the body
Based on a study, in comparison to placebo, corticosteroids improved airflow and decreased the rate of treatment failure and risk of relapse and decreased the length of hospital stay.
9) Neb with Ipravent, Budecort 6 hourly
Ipravent belongs to a
group of medicines known as anticholinergic bronchodilators, work by
relaxing the bronchial tubes that carry air in and out of your lungs and makes
breathing less difficult.
Budecort (Budesonide) belongs to a group of medicines called
'corticosteroids'. It works by reducing and preventing swelling and
inflammation in your lungs’.
Efficacy based on a study where
Patients received 2 mg of budesonide every 6 h (n = 71),placebo (n = 66). All
received standard treatment, including nebulized beta(2)-agonists, ipratropium
bromide, oral antibiotics, and supplemental oxygen. The mean change (95%
confidence interval) in postbronchodilator FEV(1) was greater with active
treatments than with placebo: budesonide versus placebo, 0.10 L (0.02 to 0.18
L)
10) Tab Pulmoclear 100 mg PO OD
Is a combination of two mucolytic medicines: Acebrophylline and Acetylcysteine.
It thins and loosens mucus (phlegm) making it easier to cough and relaxes the airway muscles and thereby promotes easy inflow and outflow of air
11) Chest physiotherapy
Chest PT expands the lungs, strengthens breathing muscles, loosens and improves drainage of thick lung secretions, thus improving lung function.
12) GRBS 6 hrly
To monitor blood sugar levels
13) Inj HAI SC
Human Actrapid Injection contains human insulin (short acting), that helps lower blood sugar levels in a diabetic patient.
14) I/O charting - Is used to record fluid intake and output
15) Inj. Thiamine 1 amp in 100 ml of NS
Based on a study- The administration of a single dose of thiamine was
associated with a trend toward increase in oxygen consumption in critically ill
patients
Thiamine deficiency is seen in
patients taking loop diuretics (lasik), as this patient is receiving LASIK, the
use of thiamine could be prophylactic.
Q3. What could be the causes for her current acute exacerbation?
ANS. The patient has three main cases that increase the chances of acute attacks of COPD,
- A history of attacks
- Being a known case of diabetes mellitus since 18 years
- Being a patient with HTN
A history of HTN will lead to an increase in the pressure of the pulmonary artery. The presenting hypoxia will further aggravate this, leading to right sided heart failure.
https://erj.ersjournals.com/content/32/5/1371)
Q4. Could the ATT have affected her symptoms? If so how?
ANS. There are some case reports about interstitial lung disease (ILD) such as pneumonitis caused by isoniazid (INH), rifampin (RFP), ethambutol (EMB). Therefore The causative drug was discontinued permanently or re-administrated after desensitization therapy. The ATT could have also been the reason for generalized weakness.
Reference- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3480752/
Q5. What could be the causes for her electrolyte imbalance?
ANS. Activation of the renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may aggravate the electrolyte imbalance during acute exacerbation of COPD.
This patient has Hyponatremia and Hypochloremia according to the reports
Hyponatremia in patients with COPD developed secondary to many reasons, such as development or worsening of hypoxia, hypercapnia, and respiratory acidosis, and right-side heart failure with development of lower limb edema, renal insufficiency, use of diuretics etc.
Respiratory acidosis with metabolic alkalosis (owing to renal compensation) in patients with COPD with chronic hypercapnia is the usual cause of hypochloremia in those patients.
2) NEUROLOGY
CASE A
Q1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS. Patient has a history of seizures. The timeline of this patient is as follows:
1 year ago- First episode of seizure
4 months ago- Second episode of seizure (24 hours after with the withdrawal of alcohol, leading to restlessness, sweating and tremors)
9 days ago- Started talking and laughing to himself, decreased food intake, unable to recognize family members, has short term memory loss.
Anatomical localization: There are lesions in
the central nervous system.
Etiology: Since the Patient has a history of consumption of alcohol, this will lead to a deficiency in thiamine. A thiamine deficiency gives rise to Wernicke’s Encephalopathy, which is the presence of neurological symptoms caused by biochemical lesions of the central nervous system after exhaustion of B-vitamin reserves, in particular thiamine (vitamin B1).
Q2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS.
a) IVF NS and RL @150ml/hr
- Normal saline and ringer lactate solutions are both crystalloid fluids. NS contains 154 mM Na+ and Cl-, with an average pH of 5.0 and osmolarity of 308 mOsm/L. LR solution has an average pH of 6.5, is hypo-osmolar (272 mOsm/L), and has similar electrolytes (130 mM Na+, 109 mM Cl-, 28 mM lactate, etc.) to plasma.
b) Inj. 1amp Thiamine in 100ml NS, TID
Thiamine is given in patients that are chronic alcoholics, due to the pathology which causes the thiamine levels in the body are deficient. Thiamine is required in the breakdown of glucose.
c) Inj. Lorazepam
- Lorazepam is mostly given to reduce the anxiety the patient feels.
- According to studies, Lorazepam has a 50% better result rate in reducing the patient’s anxiety than a placebo.
4.
d) Tab Pregabalin 75mg/PO/ BD
- MOA: Although the mechanism of action has not been fully elucidated, studies involving structurally related drugs suggest that presynaptic binding of pregabalin to voltage-gated calcium channels is key to the antiseizure and antinociceptive effects observed in animal models.
- Indication: Pregabalin is indicated for the management of neuropathic pain associated with diabetic peripheral neuropathy, postherpetic neuralgia etc and as adjunctive therapy for the treatment of partial-onset seizures in patients.
5. e) Lactulose 30ml/PO/BD
- MOA: Lactulose is a synthetic disaccharide derivative of lactose. Saccharolytic bacteria present in the large intestine subsequently break the substance down into organic acids like lactic acid. Such resultant volatile fatty acid metabolites, in combination with hydrogen and methane that is also generated consequently increase intraluminal gas formation, gut motility, and elicit an osmotic effect that facilitates an increase in the water content of stool as well as associated stool softening. All of these actions ultimately assist in facilitating and increasing the frequency of bowel movements in patients experiencing constipation.
- Indication: Lactulose is also employed as an adjunct to protein restriction and supportive therapy for the prevention and treatment of portal-systemic encephalopathy (PSE), including both the hepatic pre-coma and coma variations.
f) Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
- MOA: Supplemental potassium in the form of high potassium food or
potassium chloride may be able to restore normal potassium levels.
- Indication: For
use as an electrolyte replenisher and in the treatment of hypokalemia.
g) Syp Potchlor 10ml in one glass water/PO/BD
- It is
a supplement of Potassium, it has the above given mechanism of action and
indications.
Q3. Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
ANS. In this case, the patient mainly deals with two main neurological symptoms: seizure activity and memory loss.
Seizures: Repeated alcohol intake and
withdrawal is termed as kindling. Kindling is a process whereby there can be
small chemical and electrical stimuli which can precipitate the seizure
activity.
Memory
Loss: Alcohol may have a direct neurotoxic effect on cortical neurons,
but much of the damage may be secondary to a pre-existing pathology caused by
thiamine deficiency. Studies have shown that Wernicke Encephalopathy patients
have widespread cerebral and subcortical atrophy.
With the continuous use of alcohol, there is
a constant decrease in the levels on thiamine in the body, which gives rise to
delayed neurological symptoms.
Q4. What is the reason for giving thiamine in this patient?
ANS. A chronic alcoholic has a depleted supply of thiamine in the body, due to poor diet, which can give rise to neurological symptoms, such as Wernicke Encephalopathy. To prevent some of the symptoms, thiamine is given to replenish the supply of the patient.
Q5. What is the probable reason for kidney injury in this patient?
ANS. Mechanism for alcohol-induced kidney injury is:
Chronic alcohol consumption induces profound injury in several organs that may affect and aggravate the effect of ethanol on the kidney.
Ethanol itself markedly induces the expression of the microsomal ethanol oxidation system, producing reactive oxygen species as a byproduct. Increased gastrointestinal permeability and endotoxin load may lead to alcoholic steatohepatitis resulting in excessive immunoglobulin A (IgA) load. IgA deposits may accumulate in the kidney, leading to glomerulopathy.
Renal microcirculatory changes in advanced liver cirrhosis leads to hepatorenal syndrome. Alcohol-induced skeletal muscle damage leads to excessive amounts of circulating myoglobin, causing renal tubular injury because of increased oxidative stress.
Q6. What is the probable cause for the normocytic anemia?
ANS. The probable cause for normocytic anemia is kidney disease.
Q7. Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
ANS. Yes, chronic alcoholism could have aggravated the formation on the foot ulcer. In the case of a chronic alcoholic, there is a depression in the immune system, the same way it is for diabetics. This can also lead to alcoholic neuropathy. Alcoholic neuropathy involves coasting caused by damage to nerves that results from long term excessive drinking of alcohol and is characterized by spontaneous burning pain, hyperalgesia, and allodynia. Chronic presentation will increase the chances of foot ulcer formation and also increase the time of recovery.
CASE B
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
1) Q1. What is the evolution of the
symptomology in this patient in terms of an event timeline and where is the
anatomical localization for the problem and what is the primary etiology of the
patients problem?
ANS. Timeline of the patient is as
follows-
7 days back- Patient gave a history of giddiness
that started around 7 in the morning; subsided upon taking rest; associated
with one episode of vomiting
4 days
back- Patient
consumed alcohol; He developed giddiness that was sudden onset, continuous and
gradually progressive. It increased on standing and while walking.
H/O postural
instability- falls while walking
Associated
with bilateral hearing loss, aural fullness, presence of tinnitus
Associated
vomiting- 2-3 episodes per day, non projectile, non bilious without food
particles
Present
day of admission-
Slurring of speech, deviation of mouth that got resolved the same day
Anatomical
location- There is a
presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology- Ataxia is the lack of muscle
control or co-ordination of voluntary movements, such as walking or picking up
objects. This is usually a result of damage to the cerebellum (part of the
brain that controls muscle co-ordination)
Many
conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain
medications eg. Barbituates, stroke, tumours, cerebral palsy, brain
degeneration etc.
In this
case, the patient has hypertension for which he has been prescribed medication
that he has not taken. Stroke due to an infarct can be caused by blockade or
bleeding in the brain due to which blood supply to the brain is decreased,
depriving it of essential oxygen and nutrients. This process could’ve caused
the infarct formation in the cerebellar region of the brain, thus causing
cerebellar ataxia.
2)
Q2. What are the mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient
ANS.
A) a) Tab Vertin 8mg- This is betahistine; It is an
anti- vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the
inner ear. This leads to local vasodilation and increased vessel permeability.
This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used
due to patients history of giddiness and balance issues.
b) Tab Zofer 4mg- This is ondanseteron; It is an anti emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and
they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this
patient.
c) Tab Ecosprin 75mg- This is aspirin; It is an NSAID
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level
and thromboxane synthesis
Indications- They are anti platelet medications and in this case used to
prevent formation of blood clots in blood vessels and prevent stroke.
D) d) Tab Atorvostatin 40mg- This is a statin
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting
step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases
cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL
uptake and degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is
used for primary prevention of stroke.
E) e) Clopidogrel 75mg- It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12
receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and
stroke by preventing clotting
F) f) Thiamine- It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the
patient consumes excess alcohol- so he may get thiamine deficiency due to poor
nutrition and lack of essential vitamins due to impaired ability of the body to
absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes
encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
G) g) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
3) Q3. Did the patients history of denovo
hypertension contribute to his current condition?
ANS. A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive
responses are impaired in this case, thus leading to endothelial dysfunction in
this case. High BP can also promote cerebral small vessel disease. All these
factors contribute to eventually lead to stroke.
Q4. Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic stroke?
ANS. Meta analysis of the relation between alcohol consumption and increased risk of stroke has mainly weighed in to the formation of two types- ischaemic and haemorrhagic stroke.
Ischaemic stroke- this is more common. This Is caused by a blood clot
blocking the flow of blood and preventing oxygen from reaching the brain
Haemorrhagic stroke- occurs when an aneurysm bursts or when a weakened
blood vessel leaks, thus causing cerebral haemorrhage
According to a Cambridge study, heavy drinkers have 1.6 more chance of
intracerebral haemorrhage and a 1.8 increased chance of subarachnoid
haemorrhage. The adverse effect on BP that is seen due to increased drinking is
a major stroke risk factor and increase the risk of heart stroke.
Many studies show that with mild and moderate drinking . the risk of
ischaemic stroke decreases due to decreased level of fibrinogen which helps in
the formation of blood clots. However, heavy alcohol intake is associated with
impaired fibrinolysis, increased platelet activation and increased BP and heart
rate.
So In this case, his history of alcoholism, coupled with his hypertension
definitely could be a causative factor of his current condition.
CASE C
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
Q1. What is the
evolution of the symptomatology in this patient in terms of an event timeline
and where is the anatomical localization for the problem and what is the
primary etiology of the patient's problem?
ANS. Timeline-
1) 10 years back – episode of
right and left upper limb paralysis
2) 1 year back- right and left
paresis due to hypokalemia
3) 8 months ago- bilateral pedal
edema, gradually progressing, present in both sitting and
standing position, relieved on taking medication
4) 7 months ago – diagnosed with
infection in the blood
5) 2 months ago – visited our
hospital for neck pain and received medication
6) 6 days ago – pain in the left
upper limb, radiating along the upper limb, dragging type, nocturnal increase
in the pain, aggravated during palpitations and relieved on medication
7) 5 days ago –
i) Palpitations, sudden in onset,
more during night time, aggravated by lifting weights and speaking
continuously, relieved by drinking more water, medication
ii) Dyspnoea during palpitation (
NYHA class 3)
iii) Chest pain associated with
chest heaviness
Anatomical location- Cervical
spine
Etiology- The patient experienced episodes of
palpitations, paresis, paralysis and edema because of hypokalemia
Neck pain is due to cervical spondylosis
Q2. What are
the reasons for recurrence of hypokalemia in her? Important risk factors for
her hypokalemia?
ANS. Since the patient complains of edema, the drugs used to relieve it such as diuretics can cause hypokalaemia.
The risk factors include-
- Excess Alcohol use
- Chronic kidney disease
- Diabetic ketoacidosis
- Diarrhoea
- 5. Diuretics
- Excessive laxative use
- Folic acid deficiency
- Vomiting
Q3. What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ANS. The earliest electrocardiogram (ECG) change associated with hypokalemia is a decrease in the T-wave amplitude. As potassium levels decline further, ST-segment depression and T-wave inversions are seen, while the PR interval can be prolonged along with an increase in the amplitude of the P wave. The U wave is described as a positive deflection after the T wave, often best seen in the mid-precordial leads.
First image- ECG showing generalized deep ST depressions, T wave inversions, and ST elevation in aVR
CASE D
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
Q1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
ANS. Stroke is the most common cause of seizures in the elderly.
Stroke is of two types:
·
Hemorrhagic stroke- this occurs
as a result of bleeding within or around the brain.
·
Ischemic stroke- this occurs
as a result of blood clot or a lack of blood flow to the brain.
People who’ve had a hemorrhagic stroke are more likely to have seizures after a stroke than those who’ve had an ischemic stroke.
Seizures following a stroke (post seizure stroke) are of 2 types:
·
Early onset seizures have
peak within 24 hours after stroke.
·
Late onset seizures occur
after 2 week of stroke onset, peak within 6-12 months after the stroke has a
higher rate of recurrence
Epilepsy is a condition characterised by recurrent episodes of seizures
Pathogenesis of seizures following stroke-
Early onset seizures after ischaemic strokes are due to an
increase in intracellular Ca2+ and Na+ with a resultant lower threshold for
depolarisation.
Late onset seizures are due to glottic scarring and are associated with the persistent changes in neuronal excitability
Q2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
ANS. The patient has a history with seizure activity, so due to this there is an increase in the chemical and mechanical activity , which leads to the development of organic lesions in the brain. The bigger the lesions the more severe the symptoms.
Since this patient has had recurrent seizures (15 episodes in the
last 5 years) there might be an aggravation on symptoms during this episode
compared to the last.
This could be responsible for his
loss of consciousness.
CASE E
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Q1. What could have been the reason for the patient for developing ataxia in the past 1 year?
ANS. This patient has a history of alcohol abuse for the past three years. Excessive alcohol consumption can be a major risk factor for development of cerebellar dysfunction or cerebellar ataxia.
A potential mechanism for this is alteration in GABA-A
receptor dependent neurotransmission. Ethanol is shown to disrupt molecular
events at the mossy fibre-granule cell-golgi cell synaptic site and the granule
cell fibre-Purkinje cell synaptic site, which is mainly responsible for ethanol
induced cerebellar ataxia.
Another mechanism is the relation between age related effect
of ethanol on the endoplasmic reticulum of purkinje cells of dendrite causing
dendritic regression, and the effect of ethanol withdrawal that causes
mitochondrial damage in the cerebellum.
Ethanol also causes neuroinflammation and neurotoxicity in
the cerebellum.
These can all affect the cerebellum, which is the motor
coordination centre of the central nervous system, and also involved in
cognitive processing and sensory discrimination. These can all result in
altered hand movements, impaired postural stability and balance, loss of fine
movements etc.
ANS. This patient has a
history of excessive alcohol consumption for the past three years. According to
a Cambridge study, heavy drinkers have 1.6 more chance of intracerebral
haemorrhage and a 1.8 increased chance of subarachnoid haemorrhage. The adverse
effect on BP that is seen due to increased drinking is a major stroke risk
factor and increase the risk of heart stroke. Heavy drinking is a major cause
of the acute cerebral hemorrhage of frontal, parietal and temporal lobes in
this patient.
Bleeding diathesis is an unusual susceptibility to bleed (hemorrhage)
mainly due to hypercoagulability. Heavy drinking can cause thrombocytopenia, as
well as impact shape and functions of platelets. Impaired platelet function,
together with reduced platelet count, can contribute to this condition
associated with chronic alcoholism. This can also cause an increased incidence
and recurrence of gastrointestinal hemorrhage associated with excessive alcohol
intake.
Q1. Does the patient’s history of road traffic
accident have any role in his present condition?
ANS. https://www.ahajournals.org/doi/pdf/10.1161/01.STR.14.4.617
The above study is similar to the case discussed where an accident occurring years ago has eventually led to an infarct. Similarly, the accident that occurred in our patient 4 years ago can be the reason for his present condition.
Q2. What are warning signs of CVA?
ANS.
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body.
- Sudden confusion, trouble speaking, or difficulty understanding speech.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
- Sudden severe headache with no known cause.
Q3. What is the drug rationale in CVA?
ANS. 1) Thrombolytics- Thrombolytics restore cerebral blood flow in some patients with acute ischaemic stroke and may lead to improvement or resolution of neurologic deficits.
2) Antiplatelet therapy- Due to the thrombotic origin of AIS and the involvement of platelet aggregation in the development of said thrombus, antiplatelet drugs are indicated. The most commonly used one is aspirin (NSAID).
3) Anticoagulant therapy- Anticoagulants are a heterogeneous group of pharmacological agents that by interacting with the coagulation cascade disrupt the formation of the fibrin mesh that forms the scaffold of the clot, thus preventing the formation of a blood clot in situ, or thrombus, inside the blood vessels.
Q4.
Does alcohol has any role in his attack?
ANS. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6007300/
According to the above study, patients who consume 1-21
drinks a week, have a lower chance of developing ischemic or hemorrhagic stroke
than those who are heavy drinkers. The patient is an occasional alcohol
drinker, so the chances of alcohol affecting his attack is improbable. In heavy
drinkers, alcohol can increase the chances of both types of strokes.
Q5.Does his lipid profile has any role for his attack?
ANS. The patient has an overall normal lipid profile except for the HDL count. The HDL is 33mg/dl which is lower than the normal range (40-60 mg/dl).
HDL is known as the good cholesterol. Any decrease in the
count is an indicator that there can be a cardiovascular disorder.
Studies have
demonstrated a trend toward a higher risk of stroke with lower HDL-C. Some see
HDL-C as an important modifiable stroke risk factor. In patients with recent
stroke or transient ischemic attack and no coronary heart disease, only lower
baseline HDL-C predicted the risk of recurrent stroke.
CASE G
Q1.What is myelopathy hand?
ANS. A characteristic dysfunction of the hand observed in various cervical spinal disorders, there is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
Q2.What is finger escape?
ANS. It is one of the signs in cervical cord damage, in particular cervical myelopathy.
When patient holds fingers extended and adducted, the small finger spontaneously abducts due to weakness of intrinsic muscle.
It is a component of Wartenberg’s sign-consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi.
This commonly results from weakness of the ulnar nerve innervated intrinsic hand muscles particularly palmar interosseus muscle.
Q3.What is Hoffman’s reflex?
ANS. Also known as digital reflex/snapping reflex. It is used to examine the reflexes of upper extremities.
Procedure- The doctor carries out the test procedure by holding the middle finger at the joint closest to the fingernail, flicks the nail using the other hand.
Interpretation- If there is no movement in the index finger or thumb after this motion, the person has a negative Hoffman’s sign. If the index finger and thumb move, the person has a positive Hoffman’s sign.
A positive Hoffman sign indicates an upper motor neuron lesion and corticospinal pathway dysfunction likely due to cervical cord compression.
However, a positive Hoffman sign
can be present in an entirely normal patient. This happens in individuals
who are hyper reflexive.
CASE H
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
Q1. What can be the cause of her condition?
ANS. The patient’s GTCS episodes can be due to acute cortical vein thrombosis as seen in her MRI. Seizures are the most common symptoms of CVT.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5771304/
This
case report illustrates that CVT can occur in the setting of anaemia and
thrombocytopenia.
The above case is similar to our patient. Though
neurological manifestations are not common in iron deficiency anaemia our
patient presented with CVT. Also,
our patient had thrombocytopenia which one would have expected to cause a
bleeding tendency but paradoxically could have contributed to the development
of the venous thrombosis as explained in the article above.
The
associated symptoms such as headache and vomiting can be explained by the
midline shift.
Q2. What are the risk factors for cortical vein thrombosis?
ANS.
- Birth control or excess oestrogen use.
- Dehydration.
- Ear, face, or neck infection.
- Protein deficiencie
- Head trauma or injury.
- Obesity
Q3. There was seizure free period in between but again sudden episode of GTCS why? Resolved spontaneously why?
ANS. The patient
developed high grade fever (the patient had thrombophlebitis) with could have
been the cause of the seizures. The decrease in the fever could have resolved
the seizures.
Q4. What drug was used in suspicion of cortical
venous sinus thrombosis?
ANS. The approach to treatment includes
anticoagulation (intravenous heparin or subcutaneous low molecular weight
heparin), thrombolytics (systemic or local), and symptomatic treatment (including
antiepileptic therapy, lowering intracranial pressure, decompressive craniotomy).
3) CARDIOLOGY
CASE A
https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html
Q1.What is the difference btw heart
failure with preserved ejection fraction and with reduced ejection fraction?
ANS. Ejection fraction (EF) is a measurement of how much blood the left ventricle pumps out with each contraction.
- HF with preserved ejection fraction (HFpEF) is also known as diastolic HF. In this, muscles of the heart contract normally and the heart may seem to pump a normal proportion of the blood that enters it. However, heart muscle thickening may cause the ventricle to hold an abnormally small volume of blood (chamber hypertrophy)
Therefore, although the heart’s
output may still appear to be in the normal range, its limited capacity is
inadequate to meet the body’s requirements.
Causes- Coronary artery disease, Aortic stenosis, High blood pressure
- HF with reduced ejection fraction (HFrEF) is also known as systolic HF. In this, the heart muscle is not able to contract adequately(chamber dilatation) and, therefore, expels less oxygen-rich blood into the body. Patients with this form of the disease will have lower-than-normal left ventricular ejection fraction on an echocardiogram.
Causes- Diabetes, Hypertension,
valvular heart disease
Q2.Why haven't we done pericardiocenetis in this patient?
ANS. Pericardiocentesis is a procedure done to remove fluid that has built
up in the sac around the heart (pericardium).
It's done using a needle and small
catheter to drain excess fluid.
There are 3 approaches for needle entry - left parasternal, subxyphiod approach, left apical approach. All these require a lot of precision as they might damage the surrounding pleura, diaphragm , liver.
Pericardial effusion is mild - moderate in this patient , so symptomatic treatment was given rather than opting for an invasive procedure like pericardiocentesis which requires a lot of precision.
Risks of pericardiocentesis include- Puncturing the heart, which may require surgery to repair, Puncturing the liver, Excess bleeding, which might compress the heart and affect its normal function, Air in the chest cavity, Infection etc. if the procedure is not done properly
Also this patient has pleural effusion, this might make fluid extraction difficult without inflicting and damage as the needle is inserted very close to the lungs.
Q3.What are the risk factors for development of heart failure in the patient?
ANS.
A) Cigarette smoking
The patient is a chronic smoker (30years), which is a habit known to increase the risk of heart failure.
Mechanism- Cigarette smoking leads to impaired endothelial function via decreased nitric oxide production, pro-thrombotic state, increased oxidative stress, and activated inflammatory pathways.
Smoking, via increased oxidative
stress and inflammation, directly effects on the myocardium leading to systolic
and diastolic dysfunction.
It also promotes other heart failure (HF) risk factors including
blood pressure, increased heart rate, diabetes, and atherosclerosis.
B) Chronic alcohol consumption
Patient consumes 90ml per day for the past 30 years
Heavy alcohol consumption is associated with alcoholic cardiomyopathy, characterized by left ventricular dilation, increased left ventricular mass, and reduced or normal left ventricular wall thickness among patients with a long-term history of heavy alcohol consumption.
Based on studies alcoholic
patients with symptomatic HF had 10 years or more of exposure to heavy drinking
.
C) Hypertension and Diabetes
Diabetes results in changes in myocardial structure and function by causing disproportionate left ventricular hypertrophy and perivascular and interstitial fibrosis
These changes result in diastolic and
systolic dysfunction and increase risk of heart failure.
Hypertension increases work load on
the heart and a result there is left ventricular hypertrophy — risk of heart
failure
D) ECG reports of the patient
indicate first degree AV block.
This is associated with an
increased risk of heart failure.
Among patients with heart failure, first-degree
atrioventricular block is present
in anywhere between 15% and 51%.
E) 2D ECHO of the patient shows pericardial effusion
This increases pressure on the
heart and if left untreated will lead to heart failure.
Q4.What could be the cause for hypotension in this patient?
ANS. Hypotension in this patient could be due to combination of pericardial effusion and use of diuretic LASIX (furosemide).
The pumping ability of the heart in
this patient is compromised already. Along with this he is on a loop diuretic (causing sodium, potassium and chloride loss in the urine) and is on anti
hypertensive medication (Telma 40 mg), along with fluid restriction. All these factors might result in
Hypovolemia and thereby Hypotension.
CASE B
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html
Q1. What are the possible causes for heart failure in this patient?
ANS. The patient has
various comorbidities which could have led to a heart failure.
1. a) The patient has type 2 diabetes mellitus
Diagnosed 30 years ago and has been taking human mix trad insulin daily.
He was also diagnosed with Diabetic Triopathy (applied to diabetic patients who usually have shown, first, clinical evidence of neuropathy; then, diabetic retinitis, and, finally, the nephropathy of diabetes) indicating uncontrolled diabetes which is major risk factor for heart failure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5494155/
2. b) The patient has hypertension
Diagnosed 19 years ago which is also a risk factor for heart failure
https://pubmed.ncbi.nlm.nih.gov/31472888/
3. c) Patient is a chronic alcoholic
History of alcohol cnsumption since
40 years which is a risk factor towards heart failure.
https://www.nmcd-journal.com/article/S0939-4753(19)30360-6/fulltext
The
findings in this article provide longitudinal evidence that moderate and heavy
alcohol consumption are associated with decreased LVEF and trend towards a
higher risk of incident LV systolic dysfunction, compared to light drinkers.
4. d) Patient has CKD
The patient has elevated
creatinine and AST/ALT ratios is >2 and was diagnosed with chronic kidney
disease stage IV. CKD is also one of the risk factors for heart failure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2900793/
Q2. What is the reason for anaemia in this case?
ANS. The patient has normocytic
normochromic anaemia. It could be anaemia of a chronic disease as the patient
is diagnosed with CKD stage IV.
Chronic kidney disease
results in decreased production of erythropoietin which in turn decreases the
production of red blood cells from the bone marrow.
Patient’s with anaemia and
CKD also tend to have deficiency in nutrients like iron, vitamin B12 and folic
acid essential in making healthy red blood cells
Q3. What is the reason for blebs and non-healing
ulcer in the legs of this patient?
ANS. The most common cause for blebs and non-healing ulcer in this patient is diabetes mellitus. The wound healing can be delayed due to poor circulation, nerve damage, high blood sugar levels and poor immune system response.
CKD is also known to cause delay in healing of wounds when associated with poorly controlled diabetes, neuropathy, peripheral vascular disease etc.
Anaemia can also slow down the process of healing due to low oxygen levels. Low oxygenation also makes these patients more susceptible to wound complications.
Q4. What sequence of stages of diabetes has been noted in this patient?
ANS. There are 4 stages in type 2 diabetes
- Insulin resistance
- Prediabetes
- Type 2 diabetes
- Type 2 diabetes and vascular complications, including retinopathy, nephropathy or neuropathy and, or, related microvascular events.
The patient is diagnosed with diabetic triopathy exhibiting sequence of neuropathy, retinopathy and nephropathy
The patient has been diagnosed with diabetic retinopathy, CKD stage IV and shows signs of diabetic neuropathy such as numbness
CASE C
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
Q1. What is the evolution of the symptomology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patients problem?
ANS. Timeline of the patient is as follows-
·
1 year ago- History of shortness of breath (Grade II-
SOB on exertion); He visited the hospital where he was diagnosed to be
hypertensive (on medication)
·
2 days ago- Patient was apparently
asymptomatic 2 days ago when he developed Shortness of breath Grade II (on
exertion) which progressed to Grade IV (at rest) for which he visited local RMP
and was referred to our hospital. Patient also complains of decreased urine
output since 2 days.
·
Present day- Patient came to the hospital with SOB
grade IV (on rest) and anuria for the past one day.
Anatomical Location- Patient has an issue that was
localized as an issue in the cardiac region.
Etiology- Congestive heart failure is a chronic
progressive condition that affects the pumping power of the cardiac muscle. It
occurs if the heart cannot pump (systolic) or fill (diastolic) adequately. Loss
of atrial contraction and left atrial dilation in this case cause stasis of
blood in the left atrium and may lead to thrombus formation in the left atrial
appendage. This predisposes to stroke and other forms of systemic embolism.
2) Q2. What are the mechanism of action,
indication and efficacy over placebo of each of the pharmacological and non
pharmacological interventions used for this patient?
ANS.
a)
INJ. Dobutamine-
MOA- It is a
synthetic catecholamine, that acts on B1, B2 and alpha 1 receptors.
Indications- It is a potent inotropic agent but only causes a slight increase in heart rate. It is given to patients with acute heart failure as iv infusion. 3.6ml/hr was given to maintain the falling BP up to a MAP of 55 mmHg in this case.
b) TAB. Digoxin-
MOA- It acts on
the digitalis receptor and inhibits NA-K-ATPase, thus increasing cardiac
output.
Indications- Digitalis
is used in patients with low output failure especially when associated with
atrial fibrillation, as indicated in this case.
c) INJ. Unfractionated Heparin 5000-
MOA- At low
concentration, heparin selectively inhibits the conversion of prothrombin to
thrombin, thus preventing thrombus formation. High dose heparin has
antiplatelet action and prolongs bleeding time.
Indications-
Patient had a biatrial thrombus and in this case it was used to prevent further
thrombus formation.
d) TAB. Carvediol 3.125mg BD
MOA- It blocks B1, B2, Alpha 1 adrenergic receptors and no
intrinsic sympathomimetic activity.
Indications- Used as a long term drug to reduce mortality
in patients with congestive heart failure.
e) TAB. Acetyl cysteine 600mg PO TID
f) TAB. Acitrom 2mg OD
MOA- It is an
anticoagulant that functions as a vitamin K antagonist.
Indications- oral
anticoagulant which helps to prevent formation of harmful blood clots in the
legs, lungs, brain and heart. It is used for deep vein thrombosis, pulmonary
embolism and stroke prevention.
g) TAB. Cardivas 3.125mg PO/BD
MOA- It is
carvediol. It blocks B1, B2, Alpha 1 adrenergic receptors and no intrinsic
sympathomimetic activity.
Indications- Used
as a long term drug to reduce mortality in patients with congestive heart
failure.
h) TAB. Dytor 10mg PO/OD
MOA- It is
torsemide, a loop high ceiling diuretic. It acts on the thick ascending limb of
the loop of henle, increases Na, K and Cl excretion in the urine.
Indications- preferred in cases of hypertension associated with CCF and renal failure.
i) TAB Pan D 40mg PO/OD
MOA- It is a
combination of domperidone and pantaprazol. It is a proton pump inhibitor and
helps decrease acid production in the stomach.
Indications- used to treat gastroesophageal reflux disease (Acid reflux) and peptic ulcer disease by relieving the symptoms of acidity such as indigestion, heartburn, stomach pain, or irritation.
j) TAB. Taxim 200mg PO/OD
MOA- It is
cefixime. They are beta-lactam antibiotics that inhibit synthesis of bacterial
cell wall and produce a bactericidal effect.
Indications-
Given mainly to prevent development of bacterial infections.
k) INJ. Thiamine 100mg in 50ml NS IV/TID
It is vitamin B1. It is naturally found in many
foods in the human diet. In this case, the patient consumes excess alcohol- so
he may get thiamine deficiency due to poor nutrition and lack of essential
vitamins due to impaired ability of the body to absorb these vitamins.
l)
INJ. HAI S.C 8U-8U-6U
Insulin given in
this case to treat the patients denovo diabetes mellitus.
3)
Q3. What is the pathogenesis of renal involvement
due to heart failure (cardio renal syndrome)? Which type of cardio renal
syndrome is this patient?
ANS. Cardio renal syndrome is basically
defined as “any acute or chronic problem in the heart or kidneys that could
result in an acute or chronic problem of the other.”
The leading cause of CHF includes ischemic heart
diseases and myocardial infarction, diabetes mellitus (DM), the metabolic
syndrome and hypertension. CHF evolves due to a single cause, such as
myocardial infarction or a cumulative process of multiple minor effects. Often one
entity is poorly controlled and causes significant system stress. There is
immediate stress on the kidney through pathophysiological connections when CHF
develops. The connectivity of the vascular bed, and its regulation by the
sympathetic nervous system (SNS) and renin-angiotension-aldosternone system
(RAAS), continues the stress on the nephron. The long-term process
results in scarring and fibrosis to both organs.
CHF as a
syndrome occurs due to the over expression of biologically active molecules
that are capable of deleterious effects. The cells such as the myocardial
myocytes, are capable of producing these potentially toxic effectors within
close vicinity of the injury with the capacity for ongoing autocrine and
paracrine activity. The spill over of this toxic milieu reaches the kidney,
which has to regulate salt and water retention to compensate for loss of
cardiac output. Finally, an important source of renal stress is increased
cardiac preload.
The kidneys receive 25% of blood flow, where the majority goes to the cortex, which also has the greatest neural innervations to regulate changes acutely. The medulla receives only 10% of the blood supply. The renal microvascular bed however is continuous throughout. Thus, disease in any glomeruli could have implications when placed under supraphysiological stress from SNS or RAAS and matched with early disease in vascular endothelium and nitric oxide systems.
( Reference- https://www.ncbi.nlm.nih.gov/books/NBK542305/ )
In this case the patient has Type 4 cardiorenal syndrome: a chronic
decline in kidney function that results in chronic cardiac dysfunction.
4)
Q4. What are the risk factors for atherosclerosis
in this patient?
ANS. In this case, the risk factors for the development of atherosclerosis include:
a)
Patient has Diabetes mellitus type 2, which can
accelerate atherosclerosis by driving inflammation and slowing down blood flow.
b)
Patient has history of alcohol abuse that can lead to
atherosclerosis and increase the risk of stroke.
c)
Patient has a history of NSAID abuse, which can
change the vessels ability to relax and also stimulate growth of smooth muscle
cells inside the arteries, thus leading to the clogging of the arteries.
d)
Patient also has a history of hypertension-
effect on the arterial wall also results in the aggravation and acceleration
of atherosclerosis, particularly of the coronary and cerebral vessels.
Moreover, hypertension appears to increase the susceptibility of the
small and large arteries to atherosclerosis.
5) Q5. Why was the patient asked to get those APTT, INR tests for review?
ANS. APTT- Activated partial thromboplastin time; this is a blood test that characterizes coagulation of blood. The patient has a propensity for thrombus formation, which needs to be monitored by keeping check on the aPTT levels which is an indicator for the coagulability of the blood.
INR- It is
international normalized ratio; it is also a measure of the ability of the
blood to clot. This is an important test for patients who are on blood thinners
(ie) anticoagulants. The patient in this case was taking heparin, so everyday
reports of his INR value were needed.
CASE D
Q1. What is the evolution of the
symptomatology in this patient in terms of an event timeline and where is the
anatomical localization for the problem and what is the primary etiology of the
patient's problem?
ANS. Timeline of events-
- 12 years ago- Diagnosed with type 2 diabetes mellitus (on
medication)
- Last 1 year- Heart burn like episodes since, relieved without medication
- 7
months ago- Diagnosed with pulmonary TB; Completed full course of treatment; presently sputum negative.
- Past 6 months - Hypertension diagnosis (on medication)
- Since
half an hour- Shortness of breath, Grade IV (SOB even at rest)
Anatomical localisation - Cardiovascular system
Etiology- The patient is both Hypertensive and diabetic, both these conditions can cause atherosclerosis (there is build up of fatty and fibrous material inside the wall of arteries)
Q2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS. Pharmacological interventions:
a) TAB MET XL 25 MG/STAT
Contains Metoprolol as active ingredient
MOA: Metoprolol is a cardioselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect) and with less force (negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat
Angina, High blood pressure and to lower the risk of hear attacks .
Efficacy studies- Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Non pharmacological interventions - Advised to this patient is PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention
is a non-surgical procedure that
uses a catheter (a thin flexible tube) to place a small structure called a
stent to open up blood vessels in the heart that have been narrowed by plaque
buildup (atherosclerosis).
Q3. What are the indications and
contraindications for PCI?
ANS. Indications:
- Acute ST-elevation myocardial infarction (STEMI)
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Unstable angina.
- Stable angina.
- Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
Contraindications:
- Intolerance for oral antiplatelets long-term.
- Absence of cardiac surgery backup.
- Hypercoagulable state.
- High-grade chronic kidney disease.
- An artery with a diameter of <1.5 mm
Q4. What happens if a PCI is
performed in a patient who does not need it? What are the harms of
overtreatment and why is research on overtesting and overtreatment important to
current healthcare systems?
ANS. Although PCI is generally a safe procedure , it might cause serious certain complications like
- Bleeding
- Blood vessel damage
- Allergic reaction to the contrast dye used
- Arrhythmias
- Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it. Research on over-testing and over-treatment is important as they are more harmful than useful.
Harm to patients
- Performing screening tests in patients with who at low risk for the disease which is being screened.
- For example: Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
- Overuse of imaging techniques such as X-rays and CT Scans as a part of routine investigations.
- Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant
- Over-diagnosis through overtesting can psychologically harm the patient.
- Hospitalisations for those with chronic conditions who could be treated as outpatients can lead to economic burden and a feeling of isolation.
- The use of expensive technologies and machineries are causing economic burden on health care systems.
CASE E
Q1. What is the evolution of the symptomatology in this patient
in terms of an event timeline and where is the anatomical localization for the
problem and what is the primary etiology of the patient's problem?
ANS.
Timeline-
3 days back- Developed chest pain on the right side of the chest.
- Atherosclerosis – Also known as coronary artery disease, this
condition is the most common cause of heart attacks and occurs when the buildup
of fat, cholesterol, and other substances forms plaque on the walls of the
coronary arteries
- Coronary artery spasm – A rare cause of blockage, spasms of the
coronary arteries can cause them to become temporarily constricted.
- Coronary artery tear – Also known as a spontaneous coronary artery dissection, a tear in a coronary artery can prevent blood from reaching the heart and cause a heart attack.
·
Q2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS.
a) TAB. ASPIRIN 325 mg PO/STAT
MOA-
Aspirin is a NSAID. They inhibit COX-1 and COX-2 thus decreasing the
prostaglandin level and thromboxane synthesis.
Indications-
They are anti platelet medications and, in this case, used to prevent formation
of blood clots in blood vessels.
Efficacy over Placebo: According to the study, there was a clear reduction in some serious cardiovascular adverse events. Aspirin use was associated with a lower risk of myocardial infarction than placebo use or no treatment (risk ratio [RR], 0.83, 95% confidence interval [CI]: 0.73–0.95, P = 0.005
b) TAB ATORVAS 80mg PO/STAT
Indication: Atorvastatin is indicated
for the treatment of several types of dyslipidemias. Dyslipidemia describes an
elevation of plasma cholesterol, triglycerides and increased plasma LDL. This condition represents
an increased risk for the development of atherosclerosis. Atorvastatin is
indicated, in combination with dietary modifications, to prevent cardiovascular
events in patients with cardiac risk factors and/or abnormal lipid profiles. Atorvastatin may be used as a
preventive agent for non-fatal myocardial infarction, fatal and non-fatal
stroke etc.
MOA: Atorvastatin is a statin medication and a competitive inhibitor of the enzyme HMG-CoA reductase, an early rate-limiting step in cholesterol biosynthesis. Atorvastatin acts primarily in the liver, where decreased hepatic cholesterol concentrations stimulate the upregulation of hepatic low-density lipoprotein receptors, which increases hepatic uptake of LDL. Atorvastatin also reduces VLDL, serum triglycerides, but increases HDL Cholesterol.
Efficacy over Placebo: Out
of 18 studies done, statins were shown to help in 16 studies. The studies show
a 27% reduction in the onset of MI.
c) TAB CLOPIBB 300mg PO/STAT
MOA- Clopidogrel is metabolized to its active form by
carboxylesterase-1. The
active form is a platelet inhibitor that irreversibly binds to P2Y12 ADP
receptors on platelets. This binding prevents ADP binding to P2Y12 receptors,
activation of the glycoprotein GPIIb/IIIa complex, and platelet aggregation.
Indications-
Clopidogrel
is indicated to reduce the risk of myocardial infarction for patients with
non-ST elevated acute coronary syndrome, patients with ST-elevated myocardial
infarction, and in recent MI, stroke, or established peripheral arterial
disease.
Q3. Did the secondary PTCA do any good to the patient or was it unnecessary?
ANS. PTCA
is known to improve the patient’s vessel patency if it is done within 4 hours
of the symptom onset or if it is used as adjunctive therapy along with some
systemic thrombolytic therapy. It can restore up to 90% of the vessel’s natural
state if implemented within enough time.
Though there are certain benefits from PTCA, there are some disadvantages too. If done along with systemic thrombolytics then it can lead to a higher incidence of bleeding complications. Just PTCA alone, has not proven to show any ventricular function improvement or decreased mortality.
CASE F
https://kattekolasathwik.blogspot.com/2021/05/a-case-of-cardiogenic-shock.h
ANS. The patient presented with rapid breathing, which is an indicator of cardiogenic shock, if the patient also presents along with other signs such as cold, clammy extremities.
In cardiogenic shock, there is hypovolemia, which causes reduced perfusion to major organs in the body. When there is decreased perfusion, the body slows starts shutting down. To halt this process, iv fluids are given rapidly to continue the perfusion of fluids at the normal rate. Fluid resuscitation helps restore lost blood volume, regain tissue perfusion, and reduce mortality.
When this patient was given fluids, the
perfusion returns to normal which helps abate the shortness of breath.
Q2. What is the rationale of using torsemide in this patient?
ANS. In patients who have cardiorenal syndrome, there is a renal dysfunction along with cardiac abnormalities. In such patients there is a volume overload and heart failure, the combination of which causes increased pulmonary artery or central venous pressure with low systemic pressure that may lead to a severe compromise of the net renal perfusion pressure.
Furosemide is a commonly used diuretic to treat volume overload state in heart failure, yet it is particularly prone to the problem of diuretic resistance because of its particular pharmacokinetics. Alternatives to furosemide, such as torsemide, have been shown to have a slight advantage in selected studies because of somewhat more favourable pharmacokinetics, such as longer half life and increased bioavailability of the drug.
Q3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
ANS. Patients with cardiorenal syndrome are known to have systemic inflammation which can be drawn parallel to end stage kidney disease. Here there is an inflammation of monocytes and other inflammatory cells. This puts the patient in a immune suppressive state.
Due to this state, to reduce the chances of
infection, as a prophylactic measure, ceftriaxone might have been started.
4) GASTROENTEROLOGY (& Pulmonology)
CASE A
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
Q1. What is the evolution of the
symptomatology in this patient in terms of an event timeline and where is the
anatomical localization for the problem and what is the primary etiology of the
patient's problem?
ANS. Timeline of events-
5 years ago- An episode of pain abdomen and vomiting, treated conservatively at a local hospital.
Stopped alcohol consumption.
Symptom free for almost 3 years
2 years ago- Patient started consuming alcohol, this lead to recurrent episodes of pain abdomen and vomiting.
1 year ago- 5-6 episodes of pain abdomen and vomitings
Treated by a RMP.
1 week ago- Binge of alcohol
Since 1 week- Following this he
had pain abdomen and vomiting
Since 4 days- High grade fever with chills and rigors, Developed constipation, burning micturition associated with subrapubic pain, increased frequency and urgency.
Anatomical localisation- Pancreas and left lung
Etiology- The patient is a chronic alcoholic, episodes of abdominal pain and vomiting are following alcohol consumption. Therefore it is heavy drinking that has led to the above condition in the patient.
Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
Q2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS. Drugs used in this patient -
1) ING. MEROPENEM TID for 7 days
Meropenem is a broad spectrum carbipenem antibiotic used to treat abdominal and skin infections.
Based on study-In patients with moderate to severe intra-abdominal infections, empirical monotherapy with meropenem achieved clinical response rates ranging from 91 to 100% in 7 randomised comparative trials. Meropenem also achieved clinical response rates of over 80% in patients with severe intra-abdominal infections.
2) INJ. METROGYL 500 mg IV TID for 5 days
Composition- Metronidazole
Metronidazole belongs to
Nitroimidazole group of antibiotics, is used to treat gastrointestinal
infections, skin and blood infections.
Based on the above study
metronidazole when combined with another antimicrobial agent is more effective
in the treatment of complicated intra abdominal infections (particularly those
caused by Enterobacteriacae members as they are resistant to carbipenem).
3) INJ. AMIKACIN 500 mg IV BD for 5days
Amikacin is an amino glycoside antibiotic used in the treatment of serious bacterial infections.
All the above three antibiotics are given to control infection and prevent sepsis in the patient.
4) INJ. OCTREOTIDE 100 mg SC , BD
Octreotide is a long acting
analogue of Somatostatin
It inhibits exocrine secretion of
the pancreas, also has anti inflammatory and cytoprotective effects.
Efficacy- Octeotride based on several studies did not provide any symptomatic relief or better cure when compared to other drugs . However it played a significant role in reducing serum amylase and lipase levels.
5) INJ. PANTOP 40 mg IV , OD
Pantoprazole a proton pump
inhibitor, is known to have pancreatic anti secretory effect.
Oxidative stress is common in
acute pancreatitis- Pantoprazole
has a inhibitory effect on
hydroxy radicals ( free radicals )- thereby reduces the progression of the
disease and helps in reducing oxidative stress.
PPZ treatment also reduces tissue infiltration of inflammatory
cells and acinar cell necrosis in severe AP.
6) INJ. TRAMADOL in 100 ml NS IV,OD
Tramadol is an opioid analgesic
used to relieve severe pain in acute pancreatitis.
7) INJ. THIAMINE 100 mg in 100 ml NS IV , TID*
Vitamin B1 supplement.
As the patient is on TPN there is
a chance of B1 deficiency
Wernicke’s encephalopathy ( due
to B1 deficiency) has been noted in several cases of pancreatitis
so to prevent this Thiamine is
given as a prophylactic measure
8) TPN ( Total Parenteral Nutrition )
Method of feeding that bypasses the gastrointestinal
tract. Fluids are given intravenously to provide
nutrients the body needs. The
method is used when a person cannot or should not receive feedings or fluids by
mouth.
Parenteral nutrition is used to prevent malnutrition in patients who are unable to obtain adequate nutrients by oral or enteral routes.
My approach to this case as a treating physician-
-When the patients present with the
complaints of pain abdomen and vomiting, along with fever, burning micturition,
certain investigations must be done.
- First, a general examination must
be done, including inspection, percussion, palpation and auscultation of the
abdomen.
-Other investigations are CBP
(Complete Blood Picture ), LFT( Liver Function tests ), RFT( Renal Function
Test ) , Urine analysis, Serum amylase, ABG( Arterial Blood Gas ), Pleural
tapping.
-Some imaging studies like,
contrast enhanced CT and chest x-ray should be taken as well.
-Now depending on the diagnosis
based on the results, chemotherapy must be started. In the case of pancreatitis
in this patient, the following treatment can be given.
- Antibiotic like Meropenam or Amikacin
- Fluid levels should be
maintained with RL or NS
- Somatostatin analogue like
Somatostatin, decreases the exocrine secretion in the pancreas
- Proton pump inhibitor
-Vitamins such as Thiamine
- Anti-analgesic such as Tramadol
CASE B
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
Q1. What is causing the patient's dyspnoea? How is
it related to pancreatitis?
ANS. Pancreatitis is associated with shortness of breath. Acute pancreatitis can cause chemical changes in your body that affect your lung function, causing the level of oxygen in your blood to fall to dangerously low levels.
Acute pancreatitis is associated with release of inflammatory factors which the lungs, fluid accumulation which is also associated with pancreatitis (the patient was diagnosed pleural effusion) results in shortness of breath.
Q2. Name possible reasons why the patient
has developed a state of hyperglycaemia.
ANS. Hyperglycemia in the early phase of AP may arise from mechanisms such as uncontrolled pre-existing DM, damage to the endocrine pancreas due to severe attack of AP, and metabolic stress associated with critical illness
1. Pancreatitis damages cells that produce insulin and glucagon which are hormones that control the levels of blood sugar. Insufficiency of these hormones can lead to hyperglycaemia.
2. Patient is a known alcoholic with increased consumption since 2 months (2 litres of toddy everyday) which could also be a cause of diabetes in the patient. But the patient was never tested before he came to our OPD and did not recall any notable signs.
Q3. What is the reason for his elevated
LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
ANS. Excess alcohol consumption is known to elevate LFT’s.
Alcohol is a known hepatotoxin
which effects liver functioning and there is no certain linear relation between
the amount consumed and the stage of liver damage.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155359/
Sensitivity
and specificity of biomarkers in detecting harmful or heavy alcohol consumption
|
Biomarker |
AST |
ALT |
MCV |
CDT |
CDT + GGT |
CDT + GGT + MCV |
|
Sensitivity |
47%-68% |
32%-50% |
45%-48% |
63%-84% |
83%-90% |
88% |
|
Specificity |
80%-95% |
87%-92% |
52%-94% |
92%-98% |
95%-98% |
95% |
AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; MCV: Mean corpuscular volume; CDT: Carbohydrate-deficient transferring; GGT: Gamma-glutamyltranspeptidase
(source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155359/
)
GGT and CDT are usually taken as specific markers for ALD
Q4. What is the line of treatment in this patient?
ANS. Plan
of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood
glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
•
IVF: 125 mL/hr
•
Inj PAN 40mg i.v OD
•
Inj ZOFER 4mg i.v sos
•
Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab
Dolo 650mg sos
•
GRBS charting 6th hourly
• BP
charting 8th hourly
CASE C
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
Q1) What is the most probable diagnosis in this patient?
ANS. Differential Diagnosis:
- Ruptured Liver Abscess.
- Organized collection secondary to Hollow viscous Perforation.
- Organized Intraperitoneal Hematoma.
- Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
The
most probably diagnosis is an abdominal hemorrhage. This will give
reasoning to the abdominal distention, and the blood which is aspirated.
Common symptoms include abdominal pain, shortness of breath, chest pain, dizziness, bruising around your navel or on the sides of your abdomen, nausea, vomiting, blood in urine etc.
Q2) What was the cause of her death?
ANS. After leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
Q3) Does her NSAID abuse have something to do with her condition? How?
ANS. NSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity.
While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death.
5) NEPHROLOGY
CASE A
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
Q1.What could be the reason for his SOB?
ANS. About 2% of the body's creatine (chemical product created by muscle activity) is converted into creatinine every day and is transported to the kidneys for disposal. The kidneys function to eliminate most of the creatinine via urine. If the normal kidney function is interrupted or impaired by any disease or condition, then you may find a rise in the level of creatinine.
Normal levels of creatinine in the blood are 0.6 to 1.2 mg/dl in adult males and 0.5 to 1.1 mg/dL in adult females. This patient underwent a TURP around two months ago, post which he came back to the hospital with Hyponatremia, and elevated creatinine levels (5.2 mg/dl). These were both corrected and he was discharged.
After discharge, he came for routine testing about 1 week later, with elevated creatinine levels (6.2 mg/dl), and then presented to the hospital with SOB on exertion with a serum creatinine level raised to 10 mg/dl.
This increase in serum creatinine could have contributed to shortness of breath in the patient.
Q2.Why does he have intermittent episodes of drowsiness?
ANS. Hyponatremia occurs when the concentration of sodium in your blood is abnormally low.
In hyponatremia, one or more factors — ranging from an underlying medical condition to drinking too much water — cause the sodium in your body to become diluted. When this happens, your body's water levels rise, and your cells begin to swell.
Hyponatremia signs and symptoms pertinent to this case may include:
• Headache
• Confusion
• Loss of energy, drowsiness and fatigue
In this case, post TURP in the patient he presented to the hospital with drowsiness and excessive sleep that attenders felt difficult to wake him up from sleep and attenders were regularly monitoring his BP, which was found to be fluctuating and patient was brought to the hospital and was found with Hyponatremia, which is what may have caused his drowsiness.
Q3. Why did he complaint of fleshy mass like passage in his urine?
ANS. The patient in this case has a history of dysuria and urine is cloudy in appearance. On investigation, there is a presence of pus cells in the urine. The patient has an indication of hydronephrosis, which is a condition that typically occurs when the kidney swells due to urine failing to properly drain from the kidney to the bladder. Due to stasis of fluid, these patients become predisposed to development of urinary tract infection (UTI), which can be the cause of fleshy type masses or gritty particles in the urine.
Q4. What are the complications of TURP that he may have had?
ANS. Some possible complications may include:
• Bladder injury
• Bleeding
• Blood in the urine after surgery
• Electrolyte abnormalities
• Infection
• Painful or difficult urination
• Retrograde ejaculation (when ejaculate goes into the bladder and not out the penis)
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
ANS. According to the case history, the patient, in this case an 8 year old boy, is excessively hyperactive, impulsive, does not have proper social etiquettes as is expected of his age, too active to pay any attention at school, talk so fast that even comprehending sentences becomes quite difficult.
These issues are ongoing in the boy, and are prominent enough to be negatively affecting his daily life. This prompts one to consider the possibility of the boy having ADHD (attention deficit hyperactivity disorder), a mental health disorder that can cause above-normal levels of hyperactive and impulsive behaviors. People with ADHD may also have trouble focusing their attention on a single task or sitting still for long periods of time.
People who have ADHD have combinations of these symptoms:
• Overlook or miss details, make careless mistakes in schoolwork, at work, or during other activities
• Have problems sustaining attention in tasks or play, including conversations, lectures, or lengthy reading
• Seem to not listen when spoken to directly
• Fail to not follow through on instructions, fail to finish schoolwork, chores, or duties in the workplace, or start tasks but quickly lose focus and get easily sidetracked
• Avoid or dislike tasks that require sustained mental effort, such as schoolwork or homework.
• Lose things necessary for tasks or activities, such as school supplies, pencils, books, tools, wallets, keys, paperwork, eyeglasses, and cell phones
Signs of hyperactivity and impulsivity may include:
• Fidgeting and squirming while seated
• Getting up and moving around in situations when staying seated is expected, such as in the classroom or in the office
• Running or dashing around or climbing in situations where it is inappropriate, or, in teens and adults, often feeling restless
• Being unable to play or engage in hobbies quietly
• Talking nonstop
• Blurting out an answer before a question has been completed, finishing other people’s sentences, or speaking without waiting for a turn in conversation
• Having trouble waiting his or her turn
• Interrupting or intruding on others, for example in conversations, games, or activities
(Reference link- https://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder-adhd-the-basics/)
Before ADHD is made as a proper diagnosis, these activities can often be interpreted as the child being hyperactive, out of control, and lacking in social etiquette.
Q2. Why doesn't the child have the excessive urge of urination at night time?
ANS. The child in this case has gotten a series of tests done in order to come to a conclusion about his diagnosis.
a) They have done a complete urine exam, a urine culture and sensitivity test, and checked levels of serum electrolytes. Although the cell counts in the urine examination are normal, and there are no microorganisms after urine culture, still due to the presence of some mildly enlarged mesenteric lymph nodes on USG, there still remains suspicion of an infective etiology, including cox bacilli. However, the likelihood is less, also due to the fact that the child only feels the need to pass urine frequently during the day, with no associated pain, or positive culture reports.
b) From the history of excessive hyperactivity, impulsiveness, lacking of attentivity, a thought goes towards Attention Deficit Hyperactivity Disorder (ADHD) and in turn towards the association urination disorders. Studies indicate that children with ADHD have a higher tendency to lack bladder control, and are prompted to go to the bathroom more frequently.
c) Since the child does not get the urgency to urinate when he is asleep, there can be a chance of the manifestation being psychosomatic, or as a result of an undiagnosed anxiety disorder, or a stressor triggering this manifestation.
When you feel anxious, your body’s fear response can be triggered, overwhelming your bladder’s mechanisms for retaining urine, causing you to want to urinate. The child may be free from the triggers while asleep, especially because he does not have a history of nocturnal enuresis, thus enabling him to sleep well through the night.
Q3. How would you want to manage the patient to relieve him of his symptoms?
ANS. The diagnosis of the child is leaning towards the possibility of a psychosomatic overactive bladder, which can be triggered by various stressors or the possibility of the child having undiagnosed ADHD, a conclusion based on history of his behavior. In either of these cases, change in the daily habits and behavior, along with conservative therapy such as bladder exercises can go a long way before doing medical or surgical intervention.
a) The most common treatment options include bladder retraining and pelvic floor exercises.
- Bladder retraining involves putting the child on a “voiding schedule” where they go to the restroom to urinate on a schedule. This helps to slowly train the bladder to hold more and more urine, as it is designed to.
- Pelvic floor exercises provide a way to strengthen the muscles that are used to slow and stop the flow of urine and prevent wetting.
b) If these techniques do not work or seem to have no effect on the overactive bladder, there are some medications that can be used to calm the overactive bladder. Drugs like oxybutynin can help in controlling an overactive bladder.
c) Along with these, certain lifestyle measures can be adopted to help with an overactive bladder.
- Children with ADHD welcome easily accessible distractions. Television, video games, and the computer encourage impulsive behavior and should be regulated. By decreasing time with electronics and increasing time doing engaging activities outside the home, your child will have an outlet for built-up energy.
- Get regular, daily physical activity and exercise. This can help manage the stressors that can trigger an overactive bladder in children.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology)
CASE A
https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
Q1.Which clinical history and physical findings are characteristic of tracheoesophageal fistula?
ANS. In adults, the characteristic history is recurrent pneumonia, hemoptysis, and coughing after eating. In children, the features found in cases of congenital tracheoesophageal fistula, there is Frothy, white bubbles in the mouth, coughing or choking when feeding, vomiting, blue color of the skin (cyanosis), especially when the baby is feeding, difficulty breathing.
The physical findings are, in the presence of TEF, abdominal distention may occur secondary to collection of air in the stomach.
Q2. What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANS. Immune reconstitution inflammatory syndrome (IRIS) is a condition seen in some cases of AIDS or immunosuppression, in which the immune system begins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatory response that paradoxically makes the symptoms of infection worse.
There are chances that this patient can develop IRIS due to the patient being RVD positive. She is more susceptible to any infection and therefor prone to reinfection. To prevent IRIS, the most effective method is to involve the initiation of ART before immunosuppression is advanced. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL. Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
7) Infectious disease and Hepatology
CASE A
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
Q1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it? What could be the cause in this patient?
ANS. Patient is toddy drinker since for the past 30 years and by occupation he is a palm tree climber.
Toddy is a locally brewed beverage, which is cultivated from the fruit of the palm tree and left to ferment in clay pots. If the conditions are unhygienic it gets contaminated with bacteria, fungi, parasites.
Of particular contamination with Entamoeba Histolytica is known to cause liver abscess.
Based on his occupation the patient belongs to low socio economic group - so chances of malnutrition is more, which further favours the survival of the parasite.
Q2. What is the etio-pathogenesis of liver abscess in a chronic alcoholic patient ?
ANS. The patient has a history of consumption of alcohol ( 1 bottle per day for the past 30 years). Alcohol causes Amoebic liver abcesses (ALA) through a multitude of mechanisms:
• Alcohol induced hepatic dysfunction
• It lowers body resistance and suppresses immune mechanisms in the habitual consumers.
• Locally prepared alcohol (toddy) when brewed in unhygienic conditions may be contaminated by pathogens (In this case, E Histolytica)
• Toddy has very less alcoholic content (< 5%) - this favours the survival of Entamoeba and promotes the conversion of latent forms to virulent forms resulting in more symptomatic cases.
• Alcohol-induced hepatic dysfunction and possible suppression of amoebistatic immune mechanisms by substances in the beverages could also be attributed in the mechanism [6].
Socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
(Reference- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/ )
Q3. Is liver abscess more common in right lobe?
ANS. Liver abscess is more common in right lobe than left lobe (The involvement of right lobe to left lobe is in the ratio of 2: 1)
Liver abscess is more common in the right lobe than left lobe because-
• The right hepatic lobe receives blood from both the superior mesenteric and portal veins, whereas the left hepatic lobe receives inferior mesenteric and splenic drainage
• It also contains a denser network of biliary canaliculi and overall more hepatic mass.
Q4.What are the indications for ultrasound guided aspiration of liver abscess?
ANS. Indications for aspiration of a liver abscess include the following:
• Presence of a left lobe abscess of more than 10cm in diameter.
• Pain and impending rupture.
• Abscess that does not respond to medical treatment within 3-5 days.
CASE B
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
ANS. Amoebic liver abscess (ALA ) seen commonly in the tropics is predominantly confined to adult males, especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
However , there has emerged an abundance of data that implicates alcohol in a more causal role in facilitating the extra intestinal invasion of the infective protozoan and the subsequent development of ALA. (Ref- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6586571/ , https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/ )
Hence the consumption of locally made alcohol (toddy) is the most likely cause of Liver abscess in this patient.
Q2. How do you approach this patient ?
ANS. When patient presents with chief complaints of abdominal pain, fever -
1. Detailed history regarding each of the symptom should be taken.
2. General examination to know the overall health status should be carried out.
3. Following general examination, systemic examination should be done.
Patient’s symptoms point out to the involvement of Gastrointestinal system, therefore special emphasis should be on per abdominal examination.
4. Through history and examination , we arrive at provisional diagnosis.
5. To confirm the diagnosis, investigations, imaging tests should be taken.
6. For this patient based oh his symptomatology , the following investigations should be done.
CBP, LFT, RFT, Urine analysis
7. Imaging tests- CXR, USG abdomen.
Based on the results of these the diagnosis can be confirmed, treatment can be initiated.
This patient is diagnosed with Liver Abscess (by the above approach).
The following treatment can be given.
- In practice an empirical treatment is given to treat both amoebic and pyogenic liver abscess
- This includes use of Broad spectrum antibiotics( for pyogenic liver abscess) , Metronidazole ( for amoebic liver abscess)
- Analgesics and anti inflammatory drugs -to relieve pain and fever.
- Multivitamin supplements
- Saline infusion- to maintain fluid levels.
All the above medicines should be given for 7- 10 days.
Following this review the patient and see if there is any improvement.
USG abdomen should be done se if the abscess is resolving.
Investigations ( CBP, LFT , RFT ) should be done to check for the improvement.
If the abscess did not resolve Ultrasound guided aspiration should be done.
Q3. Why do we treat here both amoebic and pyogenic liver Abscess?
ANS. The presentation for both amoebic , pyogenic liver abscess is the same (ie) pain abdomen, fever, constitutional symptoms like nausea and vomiting , loss of appetite, in some cases there may be pulmonary symptoms.
Investigations-
There is leucocytosis, elevated alkaline phosphatase, ALT, AST
USG-a hypo echoic mass for both type of abscess.
Amoebic and pyogenic liver abscess can be differentiated only by culture and sensitivity of the aspirate obtained by USG guided aspiration of abscess.
USG guided aspiration has the following risk factors associated with it:
1) If abscess is thin walled there is a risk of rupture.
2) If abscess is on the posterior aspect of the liver, it will not be accessible.
3) There is also a risk of bleeding.
Blood culture taken prior to the administration of antibiotics is helpful for identifying the causative organism but as this patient had already taken antimicrobials before he came to the hospital, there is severe abdominal pain treatment is started immediately without a blood culture report.
Considering that it is difficult to distinguish amoebic liver abscess from pyogenic liver abscess,
We treat both forms of Liver abscess empirically using-
• Broad spectrum antibiotics- a combination of penicillin , cephalosporin, aminoglycosides
• Metronidazole- has both antibacterial and antiprotozoal activity.
( Reference- https://academic.oup.com/bmb/article/132/1/45/5677141 )
Q4. Is there a way to confirm the definitive diagnosis in this patient?
ANS. Liver abscess can be confirmed by USG Abdomen.
It presents as single/ multiple, round/ oval, hypoechoic- hyper echoic mass more commonly is the right lobe of the liver.
However USG cannot differentiate an amoebic liver abscess from pyogenic liver abscess.
For this
• Blood culture
• USG guided aspiration of the abscess should be done.
This aspirate should be subjected to antigen testing for –
Subjected to microbiological culture and sensitivity to identify pyogenic organisms.
( Reference- https://academic.oup.com/bmb/article/132/1/45/5677141 )
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology)
CASE A
http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
Q1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
ANS.
3 years ago- diagnosed with hypertension
21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
11 days ago - C/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
4 days ago-
a. Patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
b. Towards the evening patient periorbital oedema progressed
c. Serous discharge from the left eye that was blood tinged
d. Was diagnosed with diabetes mellitus
6. Patient was referred to a government general hospital
7. Patient died 2 days ago
Patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then. This resulted in poorly controlled blood sugar levels.
The patient was diagnosed with acute oro rhino orbital mucormycosis. Rhino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes. The fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA.
Q2. What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS. The management of the patient was-
1. Inj. Liposomal amphotericin B
2. 200mg Iatraconazole was given as it was the only available drug which was adjusted to his creatinine clearance.
3. Deoxycholate was the required drug which was unavailable
Along with the above mentioned treatment for the patient managing others symptoms is also done by-
I. Management of diabetic ketoacidosis –
(a) Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
(b) Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
Q3. What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
ANS. Mucormycosis may be being triggered by the use of steroids, which are life-saving drugs for severe and critically ill Covid-19 patients.
Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing.
Reference- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7599039/
9) Infectious Diseases (COVID- 19)
For this question that contains details of many of the hospitals Covid 19 patients documented over this month I have collected information adhering to the following points-
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe
3) Indicate for each patient, the day of Covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe Covid (for example, altered sensorium, hypotension etc).
I have compiled all the data collected in the form of an excel spreadsheet, so as to be able to draw a comparative analysis about the progression of disease and the outcome in various patients.
https://drive.google.com/file/d/1kltJgtrvB1pfk21ebBBGspZ1t_Wn5xHs/view?usp=sharing
10) MEDICAL EDUCATION








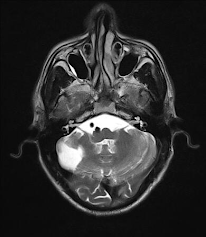
Comments
Post a Comment