Kausalya Varma, MBBS 8th semester
Roll no: 59
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 74 YEAR OLD MALE WITH SOB AND DECREASED URINE OUTPUT
CASE:
A 74 yr old male, retired RTC driver by occupation, resident of narketpally, came to the casualty with the chief complaints of fever for the past 3 days, decreased urine output for the past 2 days, shortness shortness of breath for the past 1 day.
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 3 days ago, when he developed a fever that is sudden in onset, associated with chills. It increases during nights and is relieved on medications. Fever spikes increased after connecting a urine bag 2 days ago.
He also complained about decreased urine output. Normal frequency was 4 times per day and 3 times per night. Since the past 2 days (since Tuesday morning) the output decreased. They went to local RMP at night 10pm of Tuesday & urine bag was connected by the local RMP.
Patient also complained of shortness of breath for the past day that was present at rest as well as when he was walking.
PAST HISTORY:
Medical history-
Patient was apparently asymptomatic 2 months back (in august) when he came to the casualty with the complaints of generalised body pains, vomiting, slurring of speech and not being able to swallow solids or liquids.
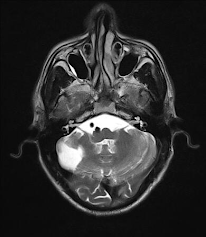
He was diagnosed in our hospital with left sided facial nerve palsy, peripheral neuropathy, denovo HTN, Spondyloarthropathy with radiculopathy sacroileitis cervical OPLL ( Ossification of posterior longitudinal ligament) and Ankylosing spondylitis.
He is a known cases of Diabetes mellitus type 2 for the past 20 years.
Patient has had cervical spondylitis for the past 10 years.
He used TB medication for a period of 18 months. He used the medications for 5 months before he developed diminished vision that was regained after 2 months.
Decreased ambulatory movements, the patient was mostly confined to a bed and has been walking with a stick for the past 1 year.
The patients past history and treatment plan was recorded and logged by an intern in Gen Med at the time. The link to the elog is given below
Surgical history- No relevant surgical history
PERSONAL HISTORY:
Diet- Vegetarian
Appetite- Decreased since past 1 month
Sleep- Decreased since past 2 days
Bowel and Bladder movements- Urine output decreased for past 2 days.
Addictions- Pateint was a chronic smoker, with a history of smoking present since 20 yrs (3 packets/day) and he stopped 5 years ago.
GENERAL EXAMINATION:
The patient was conscious, coherant, and co-operative and well oriented to time, place and person. He is sitting comfortably on the bed, moderately built and well nourished.
Pallor- Absent
Icterus- Absent
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM- Normal vesicular breath sounds heard
CVS- S1 and S2 heard, no added murmurs
PER ABDOMEN- Soft and tender, pain is present, No organomegaly, abdominal distension present
CNS- FNAD
PROVISIONAL DIAGNOSIS:
Acute Kidney Injury (Prerenal/Renal) on Chronic Kidney Disease in a patient who is a known case of HTN, DM, cervical spondylosis, ankylosing spondylosis.
Altered sensorium secondary to metabolic causes (hepatic/uraemic?)
TREATMENT:
DAY 0
1.IVF NS & RL @ 100ML/HR
2.INJ PIPTAZ 4.5 gm IV STAT
INJ PIPTAZ 2.25GM IV TID
1_______X________1
3.INJ PAN 40 MG IV OD
8AM _____X
4.INJ ZOFER 4MG/IV/SOS
5.INJ PCM 1GM IV SOS(IF TEMP >101°F)
6.INJ NORAD INFUSION( 2 AMP IN 46ML NS) @ 8ML/HR
7.BP CHARTING 2ND HRLY
8.TEMP/PR/BP CHARTING 2ND HRLY
9.INJ HAI SC (8AM__1PM___8PM)
10.GRBS CHARTING 6TH HRLY
( 8AM__1PM___8PM__2AM)
Nephrology referral
Hemogram
Serum electrolytes
Serum creatinine
Blood urea
2D Echo results
ABG
Chest X-ray
ECG- Done at 7:45pm
ECG- Done at 10:40pm
ECG- Done at 12:40pm
DEATH SUMMARY:
- A 74 year old male, came to casualty with chief complaints of Shortness of breath, with pulse not palpable, Blood pressure not recordable.
- ABG showing metabolic acidosis. Bicarbonate correction was given to the patient. Fluid resuscitation was planned.
- Triple lumen catheter ionotropic support was started with noradrenaline, dobutamine titrated to requirement.
- Nephrology opinion was taken in view of increased urea & creatinine levels, and dialysis was advised around 7 pm.
- CPR was initiated, patient was revived, the ABG showed severe metabolic acidosis.
- Ventilator settings were MODE: ACMV- VC, FiO2: 100%, PEEP: 5 cm H2O, V : 50 ml.
- Around 1:25 am patient became unresponsive. BP was not recordable, pulse not palpable. CPR was initiated according to AHA guidelines.
- Despite the above resuscitation efforts, pateint could not be revived & declared dead on 22/10/21 at 2:01am.
Immediate cause of death- Refractory hypotension, metabolic acidosis with type 1 respiratory failure.
Antecedent cause of death- AKI (intrinsic) on CKD with metabolic encephalopathy (Hepatic/uraemic?) post CPR status k/c/o T2 DM & HTN














Comments
Post a Comment