Kausalya Varma, Intern
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
40 YEAR OLD MALE WITH FEVER AND VOMITINGS
CHIEF COMPLAINTS:
A 40 year old male came with the chief complaints of fever since 1 days and vomiting since 1 day.
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 2 days back then he developed fever with chills and rigor sudden in onset and continuous in nature
Not relived on medication
H/o vomiting associated with nausea since yesterday, which had food particals as content, was non bilious and non projectile type
No h/o burning micturition
No h/o rash
No H/o abdominal pain and distension
No h/o diarrhoea
No h/o neck rigidity
No h/o night sweats
No h/o weight loss
He visited local hospital in chitiyal on the day of fever where the medication were given and the fever didn’t relieve.
PAST HISTORY-
No similar complaints in the past
Not a known case of DM, HTN, asthma, thyroid, epilepsy, CAD
FAMILY HISTORY
Not significant in this case
PERSONAL HISTORY
Diet- Mixed
Appetite- Normal
Bowel and bladder-regular
Sleep- adequate
Addictions-consumes alcohol and toddy occasionally
GENERAL EXAMINATION
Patient is conscious coherent cooperative well oriented to time place and person moderately built and nourished
Patient was examined in well lit room and consent was taken
Vitals
Pulse rate- 72bpm
B.P - 110/80
R.R 20/ min
Temp-
SpO2-92%
No signs of
Pallor icterus
Cyanosis
Clubbing
Lymphadenopathy
Edema
SYSTEMIC EXAMINATION
Per abdomen-
On inspection shape-normal
Umbilicus central
No visible scars
No engorged veins
All quadrants equally move with respiration
No visible pulsations
Palpation- All inspectory findings are confirmed
Soft and non tender
No organomegaly
No rigidity
Percussion- No fluid thrill
Auscultation- bowel sounds are heard
Respiratory system-
ON inspection trachea, scar on right upper part of chest
Palpation bilateral symmetrical expansion of chest
Auscultation- normal vesicular breath sounds
Cardiovascular system-
Inspection - No scars or engorged veins
Palpation apex beat felt
Auscultation- S1 S2 heard No murmers
CNS-
Patient is consious coherent cooperative well oriented to time place and person.
Cranial nerves - intact
Sensory system- normal
Motor Tone power bulk reflexes are normal in all 4 limbs
Fever chart-
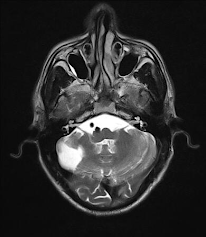
INVESTIGATIONS
DIAGNOSIS
Fever under evaluation with thrombocytopenia and hypotension
DIAGNOSIS
IV fluids (NS,ringer lactate)
Inj.neomol
Tab dolo
Plenty of oral fluids
Tepid sponging
Inj monocef
Inj.Falcigo
















Comments
Post a Comment