A 49 year old male with Viral pneumonia secondary to COVID-19
Kausalya Varma, MBBS 8th semester
Roll no: 59
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 49 year old male with Viral pneumonia secondary to COVID-19
Following is the view of my case (history as per date of admission):
Pallor- Absent
Icterus- Absent
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
Malnutrition- Absent
Dehydration- Absent
VITALS (on admission):
Temperature- Febrile (102 F)
BP- 120/80 mm Hg
Pulse- 103 bpm
Respiratory Rate- 30 cpm
Oxygen saturation- 90% on room air, 96% on 8L of O2
GRBS- 230 mg/dl
RESPIRATORY SYSTEM-
- Dyspnea is present
- Position of the trachea is central
-Vesicular breath sounds are present
- Adventitious sounds- Right sided crepitus is heard in ISA and IAA.
CVS- S1 and S2 heard, no added murmurs
PER ABDOMEN- Soft and tender, No organomegaly
CNS-
- Level of consciousness- E3V1M1; The patient is drowsy
- Pupillary and corneal reflexes are present
- Pupils reacting normally to light
- Dolls eye- positive
- Speech- patient is non responsive
- Glasgow Coma Scale- E3V1M1
- Motor system examination:
Power-
|
|
RIGHT |
LEFT |
|
UPPER LIMB |
1/5 |
1/5 |
|
LOWER LIMB |
1/5 |
1/5 |
|
|
BICEPS |
TRICEPS |
SUPINATOR |
KNEE |
ANKLE |
|
RIGHT |
+ |
+ |
+ |
+ |
+ |
|
LEFT |
2+ |
2+ |
2+ |
2+ |
+ |
The following investigations were ordered- Hemogram, RFT, LFT, MRI Brain, HIV, HBsAg, HCV
INVESTIGATIONS-
1) RFT-
Creatinine- 0.7 mg/dl
Phosphorous- 2.0 mg/dl
Sodium- 131 mEq/L
2) LFT-
Total bilirubin- 2.03 mg/dl
Direct bilirubin- 0.78 mg/dl
SGPT (ALT)- 93 IU/L
Alkaline Phosphate- 154 IU/L
Total proteins- 5.7 g/dl
Albumin- 3.12 g/dl
7) Color Doppler 2D Echo-
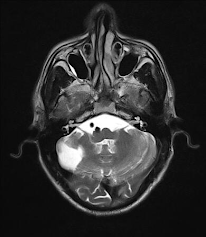
- Observed- Symmetrical foci of restricted diffusion in bilateral frontoparietal parasagittal areas.
These are suggestive of Acute bilateral parasagittal frontoparietal infarcts (watershed infarcts)
- Also seen are old infarcts with encephalomacic changes and surrounding gliosis in right frontal and parietal lobes.
FINAL DIAGNOSIS-
Severe COVID-19 Pneumonia and Hypoxic Ischaemic Encephalopathy
S/P- CABG
Heart Failure with Mid range ejection fraction
TREATMENT HISTORY-
The patient was admitted to the COVID-19 ICU, where he was continuously monitored and his treatment was recorded in the form of progress notes by the doctors in charge.
The treatment timeline is as follows-
On 12/05/21 (6:45pm)
- The provisional diagnosis is viral pneumonia secondary to COVID-19 infection.
- Suspecting viral encephalitis/ Hypoxic Ischaemic Encephalopathy with old infarcts in the right frontal and parietal lobes with post PTCA LAD territory (2012) with type 2 diabetes mellitus.
O/E- Patient is unconscious
Pulse- 122 bpm
SpO2- 86 on 15lt O2
RR- 46cpm
Non responsive to commands/pain- E1V1M1
Rx-
- O2 inhalation to maintain SpO2 > 90% (Intermittent BiPAP)
- Inj Ceftriaxone 1g IV/BD
- Inj Pantop 40mg IV/BD
- Inj Levipril 500mg IV/BD
- Tab Ecosprin 75mg OD
- Tab Clopidogrel 75mg OD
- Tab Atorovas 40mg OD
- Duolin, Budecort nebulisation every 6 hours
- GRBS every 6 hours
- Inj HAI 8am-2pm-8pm
- Temp charting 4 hourly
- Watch for seizure attack
- Monitor PR, BD, SpO2 every hour
- Inj Dexamethasone
- Inj Neomol 1mg TV TID
- Temp Charting every 4 hours
On 12/05/21 (8:00pm)
- The patient had progressive breathlessness since morning
- MRI Brain revealed B/L acute fronto parietal infarcts; features suggestive of metabolic encephalopathy (Hypoxic Ischaemic Encephalopathy)
- Airway- patent
- Breathing- Spontaneous
- Circulation- PR- 116bpm, BP- 130/70mmHg
- RR- 53cpm; SpO2- 60% with room air and 85-87% with face mask
- GCS- E1V1M1
- Temp- 104.5 F
- LP for CSF analysis was attempted but could not be done
- Ryles tube was inserted
Rx-
- O2 Therapy via a face mask
- Inj Dexamethasone 6 hourly IV TID
- Inj Neomol QID
- Temp charting 4 hourly
On 13/05/21 (9:00am)
- Patient is unconscious
- GCS- E1V1M1
- PR- 114bpm, BP- 80/60mmHg
- O2 Saturation- 81% on 16L of O2
Rx-
- Inj Levipil 500mg/BD
- Ryles tube insertion
- Tab Ecosporin 75mg/OD
- Tab Clopidogrel 75mg/OD
- Tab Atorovas 40mg
- BP, PR, Temp should be monitored hourly
- Inj PAN 40mg IV/OD
- Inj Mannitol 100mg IV/OD
- Inj HAI
- Inj Dexamethasone 6mg IV TID
- RT feed <100ml of milk and protein powder- every 2 hourly
- O2 Inhalation via face mask
- Inj Neomol 1g IV TID
- Temp charting hourly
- Tepid sponging
On 13/05/21 (evening)
Unfortunately, the patient had passed away on 13/05/21 evening, two days after getting admitted.
Death notes-
- Since admission, the patient was diagnosed with Hypoxic ischaemic encephalopathy with COVID-19 severe pneumonia. Patient was admitted to the ICU and was administered O2 therapy; SpO2 with 16lt O2 was 80%; Respiratory rate was 60cpm from the day of admission.
- The patient suddenly collapsed at 5:10pm.
- Pupils were fixed and dilated
- ECG showed flat line at 5:21pm
- Immediate cause of death- Sudden cardiac arrest due to Hypoxic Ischaemic Encephalopathy.
- Antecedent cause of death- COVID-19 Pneumonia
QUESTIONS-
1) What do you think are the factors in this patient that contributed to his increased severity in symptoms?
2) What is the relationship between ACS and the progression of COVID in this case? Could it have been a driving factor in increased severity of symptoms?














Comments
Post a Comment